The levels of E/M services are based on four types of history (Problem Focused, Expanded Problem Focused, Detailed, and Comprehensive). Each type of history includes some or all of the following elements:
Chief complaint (CC);
History of present illness (HPI);
Review of systems (ROS); and
Past, family and/or social history (PFSH).
The extent of history of present illness, review of systems, and past, family and/or social history that is obtained and documented is dependent upon clinical judgment and the nature of the presenting problem(s).
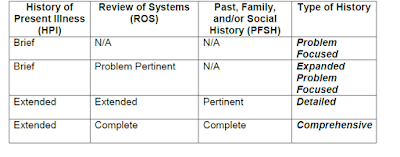
The chart below shows the progression of the elements required for each type of history. To qualify for a given type of history, all three elements in the table must be met. (A chief complaint is indicated at all levels.)
*DG: The CC, ROS and PFSH may be listed as separate elements of history, or they may be included in the description of the history of the present illness.
*DG: A ROS and/or a PFSH obtained during an earlier encounter does not need to be re-recorded if there is evidence that the physician reviewed and updated the previous information. This may occur when a physician updates his/her own record or in an institutional setting or group practice where many physicians use a common record. The review and update may be documented by:
o describing any new ROS and/or PFSH information or noting there has been no change in the information; and
o noting the date and location of the earlier ROS and/or PFSH.
*DG: The ROS and/or PFSH may be recorded by ancillary staff or on a form completed by the patient. To document that the physician reviewed the information, there must be a notation supplementing or confirming the information recorded by others.
*DG: If the physician is unable to obtain a history from the patient or other source, the record should describe the patient's condition or other circumstance which precludes obtaining a history.
*Definitions and specific documentation guidelines for each of the elements of history are listed below.